“ACEs” are traumatic events that occur between birth and age 18 that can have lasting effects on health, behavior, and overall life outcomes. The ACE study, conducted in 1998 by the Centers for Disease Control and Prevention (CDC) and Kaiser Permanente, revealed a strong connection between childhood trauma and adult health, demonstrating that preventing and mitigating ACEs is a critical public health priority (CDC, 2024). The effects of ACEs are wide-ranging and long-lasting, influencing physical health, mental well-being, and social functioning across the lifespan. These outcomes are largely driven by toxic stress, a chronic activation of the body’s stress response, which can disrupt healthy brain development and negatively affect multiple bodily systems.
61% of individuals experienced at least one ACE between the ages of 0-18 years old (CDC, 2024).
Physical Health Impacts
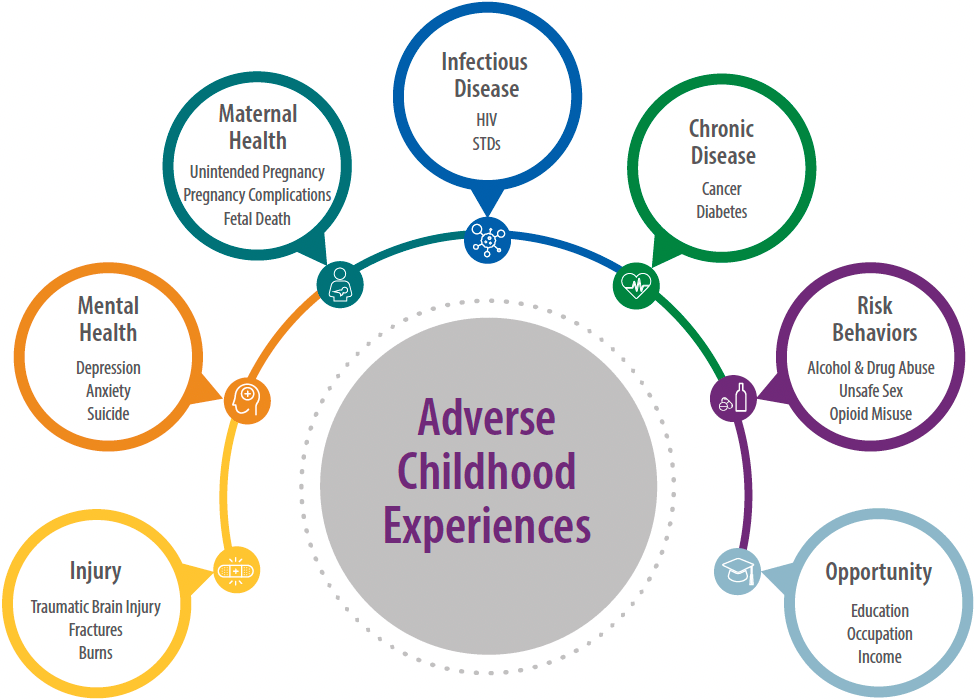
Increased risk for chronic diseases (heart disease, diabetes, cancer, stroke). Higher rates of obesity, autoimmune disorders, and sleep disturbances. Those with 6 or more ACEs may live up to 20 years less than those with none (CDC, 2024)
Mental Health Impacts
Elevated risk for depression, anxiety, PTSD, and suicidal ideation. Greater likelihood of substance use disorders and addictive behaviors. Increased rates of self-harm, eating disorders, and personality disorders (CDC, 2024)
Cognitive Impacts
Impaired learning, memory, and executive functioning. Delays in language and social-emotional development; increased likelihood of academic struggle.
Social and Behavioral Outcomes
Higher likelihood of juvenile delinquency and adult incarceration. Difficulty forming and maintaining healthy relationships. Increased risk for unemployment, homelessness, and poverty.
Prevention and Trauma Care
Preventing and mitigating the effects of Adverse Childhood Experiences (ACEs) requires a multi-level approach focused on early intervention, trauma-informed care, and resilience-building.
Prevention: Strengthen economic supports for families (housing, food, medical, and childcare assistance). Promote positive parenting programs and caregiver education. Expand community partnerships and resources for families.Increase access to high-quality early childhood education and home visitation programs (NCSTN, 2021).
Early Identification: Screen for ACEs and trauma in healthcare, school, and social service settings. Provide parent training, family therapy, and support groups for families experiencing adversity. Implement mental health programs and trauma-informed practices in schools, healthcare, and social service settings (NCTSN, 2021).
Reduction of Long-Term Effects: Deliver trauma-focused treatment and evidence-based interventions for children, adolescents, and adults. Provide wraparound support, including case management, peer support, and community-based services. Address co-occurring issues such as substance use, housing instability, or juvenile justice involvement (NCTSN, 2021)
Evidence-Based Practices
Individual Level:

Parent-Child Interaction Therapy (2-7 year olds and caregivers): Strengthens parent-child attachment and improves behavior while addressing trauma responses
Trauma-Focused Cognitive Behavioral Therapy (TFCBT): Combines cognitive-behavioral techniques with caregiver involvement to reduce PTSD symptoms, depression, and anxiety.
Dialectical Behavior Therapy (DBT): Good for expanding coping skills, mindfulness, distress tolerance, and emotional regulation skills.
Community Level:

Trauma-Informed Care (TIC): A framework across healthcare, schools, and social services that emphasizes safety, trustworthiness, collaboration, empowerment, and cultural responsiveness.
Wraparound Services: Comprehensive, individualized care coordination integrating mental health, social services, and educational support.
Positive Behavioral Interventions and Supports (PBIS): School-based approach to improve social, emotional, and academic outcomes while reducing disciplinary actions.